Latest DDD-exit: Radioactive antibody for treatment of aggressive cancer
A new antibody might be the first effective treatment for Anaplastic thyroid cancer (ATC), a very aggressive cancer type with a median survival of only 4-5 month even with available treatments. The radiolabeled antibody is the result of a four-year long successful collaboration between SciLifeLab researcher Marika Nestor (Uppsala University) and the SciLifeLab Drug Discovery and Development (DDD) platform.
It all began when Marika discovered by chance that one of the antibodies she was working on bound to ATC cells. She tasked a pathologist to look into the target expression in patient samples, who confirmed that the target was highly expressed in ATC. The target epitope is located on a membrane-bound protein called CD44v6, that is almost exclusively found on cancer cells, making it an ideal drug target. Marika immediately realized the potential in using the antibody for a potential treatment of ATC and began the search for an even better antibody together with her Ph.D. student Anja Mortensen.
At a meeting, organized by the Swedish cancer society, Marika decided to mention the project briefly, and was after the meeting approached by Fredrik Frejd (Uppsala University), Adjunct professor at the Department of Immunology, Genetics and Pathology, and CSO at Affibody. Fredrik was impressed with the project and urged Marika to prioritize the project aiming for clinical trials. Especially due to the extremely poor prognosis and the total lack of viable treatments for ATC patients.
This is when they reached out to the SciLifeLab DDD-platform and a 4-year long collaboration began.
At the time, the DDD-platform had an open national call for testing of their antibody library and a suitable antigen/epitope was required. This was perfect for Marika and her colleagues, who already had a very strong antigen candidate and needed an antibody that would be suitable to develop and translate into clinical trials. The DDD antibody platform was an ideal choice for that purpose.
Localized radiotherapy
In order for the antibody to kill tumor cells, a radioactive isotope (lutetium-177) is attached to the antibody. Since the protein containing the epitope is overexpressed mainly on cancer cells, this will create a localized radiotherapy effect, mostly affecting the cancer cells. The antibodies are injected directly into the blood stream, were they will accumulate on and around cancer cells in both the main tumor and in potential metastases.
Close collaborations
During the four-year project, Marika and her team were working closely together with the DDD-platform, carefully discussing each move before moving on to the next step.
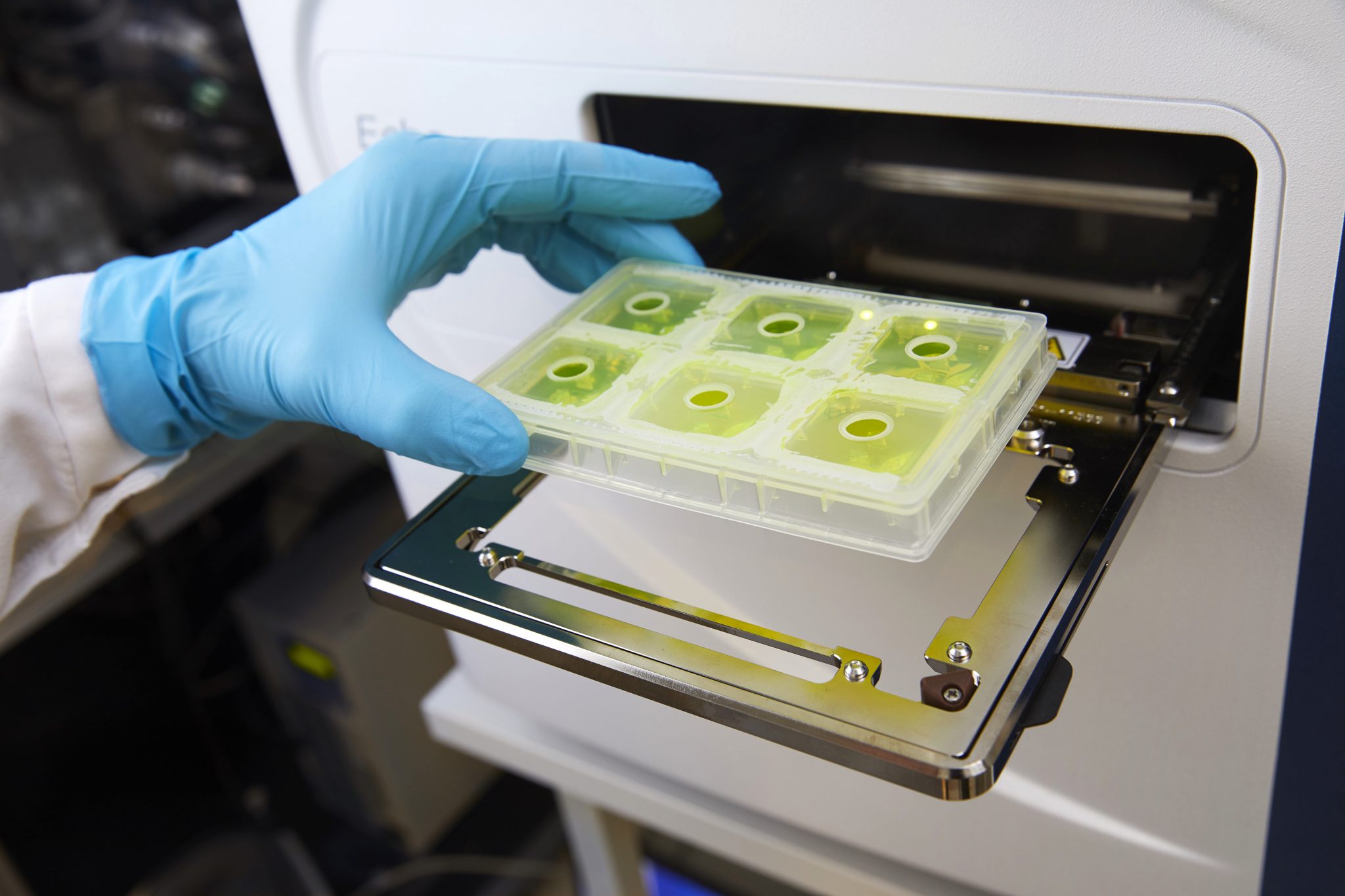
The DDD-platform helped with the selection and characterization of antibodies, stability analysis, epitope mapping, and cross-reactiveness testing, while Marika’s team could focus on cell studies, in vivo testing, and radioactive isotope selection. During these studies, Marika and her team were able to show that mice treated with the antibody could be completely cured from the cancer.
Other important properties for clinical translation of the antibody were also taken in consideration, such as the plasma half-life, potential for immunogenicity, affinity, which determines how long they will stay bound to the tumor cells, stability and production scalability. A large number of different combinations of these properties were tested in order to determine the optimal therapeutic candidate.
“I am extremely impressed with the professional level with which the SciLifeLab DDD employees ran the project. They have shown, with great industrial competence, that they can create a product that exhibits the drug-like properties that are necessary to achieve clinical studies. Not just an antibody, but also a real drug candidate”, says Fredrik Frejd.
Both Marika and Fredrik views this as an exceptionally good collaboration between the PI and the DDD-platform, where both parties have worked together as a team and utilized each other’s competence and expertise to reach clinical trials.
Funding, partners, and the future
In parallel to identifying a promising antibody candidate, Marika’s team applied for funding, which they received from e.g. Vinnova, The Swedish Society for Medical Research, and the Swedish cancer society. They also up-scaled the production of the antibody at Testa center, where more than 1 gram of antibody was obtained for use in the toxicology studies, funded by Novo Nordisk Fonden and Innopharma,. Toxicology studies has so far shown very promising results, with very little radioactivity accumulated in healthy tissue.
Marika and her team have already met with representatives from the Swedish Medical Products Agency and are currently looking for financing of the high production cost of the GMP antibody production needed for clinical trials. They have also started a new company, Akiram Therapeutics AB, as a vehicle to make the translation of the antibody drug to the patients as efficient as possible.
“We already have a medical team at Karolinska Institutet, ready to treat patients when we are ready. The project has also received very positive feedback from the Swedish Medical Products Agency, bringing our drug candidate one big step closer to the clinic”, says Marika Nestor.
“The patent is pending and we hope that we will be able to start phase one clinical trials next year”, she concludes.
“Marika and Fredrik are running a scientifically solid drug discovery project with extreme medical need. Patients affected by the disease have contacted the SciLifeLab DDD platform and Marika directly to learn more and we have been able to convey some hope for the future. I truly hope that this project can make a change for these patients”, says Kristian Sandberg, Director at the SciLifeLab DDD-platform.