Modified T-cells target Glioblastoma in latest SciLifeLab Drug Discovery and Development platform exit
The latest project to pass through the SciLifeLab Drug Discovery and Development platform (DDD) aims to find an effective treatment for Glioblastoma, an aggressive type of incurable brain cancer. The researchers are using the patient’s own T-cells modified to target tumors.
“Our ambition is to start clinical studies within four years,” says Magnus Essand (SciLifeLab/Uppsala University), in a press release from Uppsala University.
Immunotherapy, a method in which the body’s own immune system is utilized against diseases such as cancer, is a research field quickly gaining popularity. CAR T-cells, which are T-cells equipped with chimeric antigen receptor antibodies (CARs) designed to recognize specific tumor cells, were approved as a treatment of lymphoma and acute lymphoblastic leukemia in 2017. Now, Uppsala University researchers Magnus Essand and Di Yu are hoping to use the same treatment for Glioblastoma.
“The method uses the body’s T-cells and their ability to kill tumor cells. Our ambition is to extract T-cells from the patient, add a chimeric antigen receptor, a so-called CAR, and then reinsert them back into the patient. The CAR will in this case be trained to selectively recognize Glioblastoma cells. Development of a CAR T-cell product is a demanding process, one we embarked on several years ago. The results are still looking promising as we now enter the last pre-clinical phase”, says Magnus Essand.
When the group started to collaborate with SciLifeLab’s Drug Discovery and Development Platform (DDD), a national resource that assists Swedish researchers with developing new substances with the prospect of being converted into future drugs, a major step forward was taken. The joint CAR T-cells for the treatment of Glioblastoma project was launched in December 2017 and recently resulted in the submission of a patent application.
“The research group presented a high-quality project organization, one that our platform has chosen to prioritize through to the end. To use our expertise in the field of antibodies and apply it to CAR T-cells was a new experience for us, one which has given us important knowledge in advanced cell therapy. I am personally very impressed by the research team’s commitment and will follow their continued work with great interest”, says Vendela Parrow, project manager at SciLifeLab’s DDD Platform.
After two and a half years of solving problems and detailed dialogue with the DDD staff, the project was completed on June 3, 2020. A USB memory stick, containing all the research data, was handed over to the researchers at a symbolic meeting that took place at Navet, SciLifeLab’s hub in Uppsala. Both parties emphasized the synergistic effects and productivity of the collaboration.
“To have access to the expertise and techniques provided by the DDD was critical for us in order to be able to advance our research. The fact that their team has been exceptionally clear in their communication around their progress within the project has made this a very educational time for me”, says graduate student Tina Sarén (Uppsala University), one of the researchers engaged in the project.
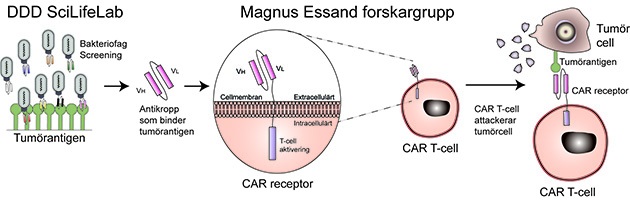
An antibody that binds to a tumor antigen expressed by glioblastoma cells was developed and a chimeric antigen receptor (CAR) was created by coupling the antibody to a T-cell receptor. T-cells that carry the CAR will thereby recognize and kill Glioblastoma cells.
Magnus Essand’s and Di Yu’s team will now validate their results for further development. At the current pace, they hope to be able to take the step to clinical studies within the next four years.
“Extremely few breakthroughs have been made around treating Glioblastoma. The tumors give rise to severe symptoms and the average survival expectancy after a diagnosis is only slightly above one year. Creating a cure is still far off, but I hope that within the foreseeable future we can offer a therapy that lengthens as well as improves the quality of life for Glioblastoma patients”, says Magnus Essand.
Photo: Private, fr Giulia Saronio, Magnus Essand, Tina Sarén, Di Yu, Vendela Parrow and Annette Roos