New type of drug candidate accelerates wound healing in first clinical study
Difficult skin wounds are an escalating silent pandemic, at the moment, only two drugs are approved. In a clinical study, researchers from SciLifeLab and Uppsala University reported that treatment using modified lactic acid bacteria performs well and has beneficial effects on wound healing.
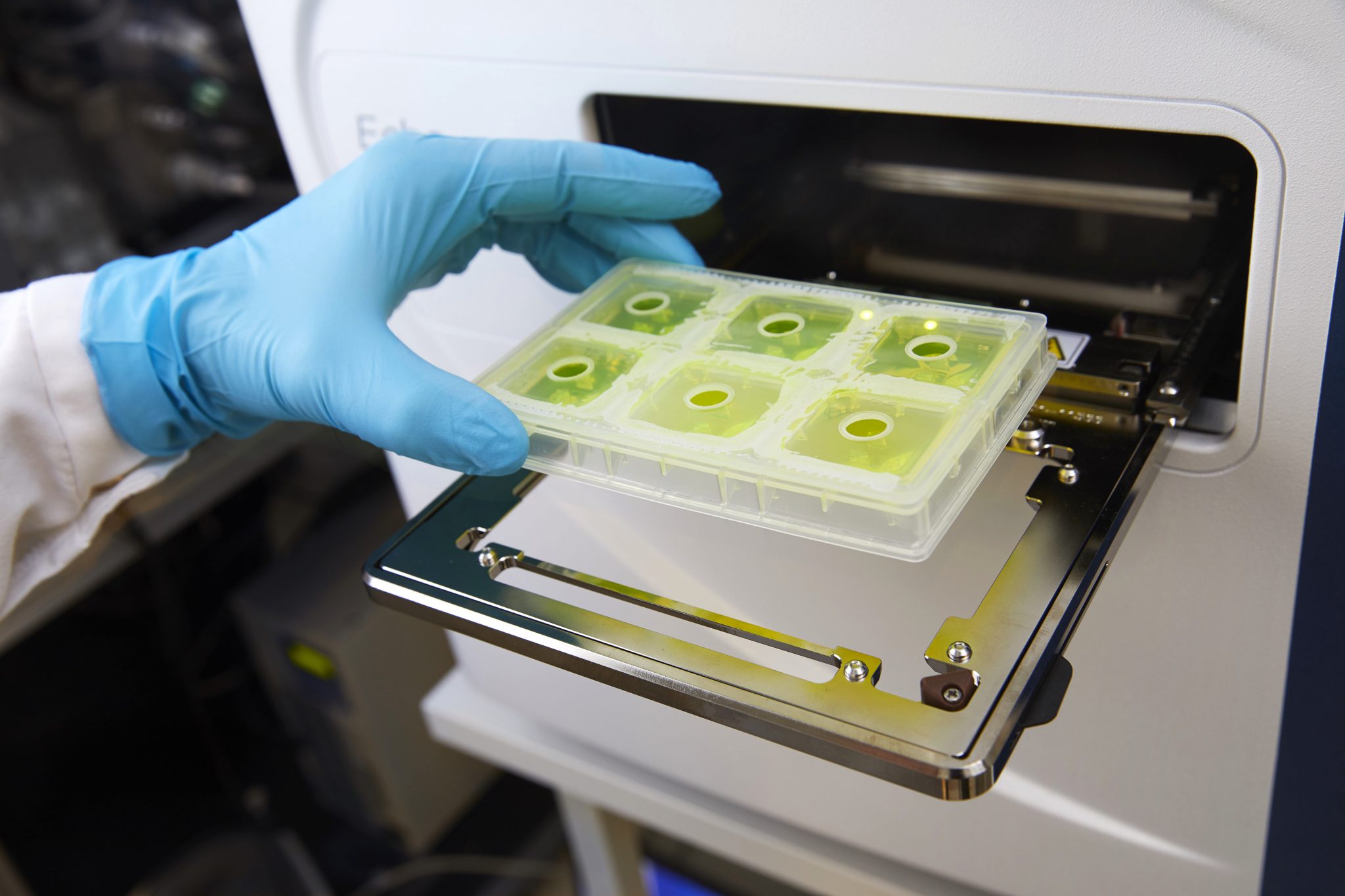
The research team responsible for this new study has previously in several controlled preclinical models demonstrated that accelerated wound healing follows topical treatment (treatment on the skin) with lactic acid bacteria genetically modified to produce the chemokine CXCL12 (ILP100-Topical). Several of the SciLifeLab infrastructure units have contributed to the research leading up to this clinical study, including Affinity Proteomics, Genomics, and the National Bioinformatics Infrastructure (NBIS).
The researchers have now published the results from the first clinical trial with ILP100-Topical (the SITU-SAFE trial) where the main objective was to establish safety and tolerability. Other aims were to assess clinical and biological effects on wound healing using traditionally accepted methods in parallel to exploratory and traceable measurements.
“We wanted to conduct a more thorough analysis which included detailed, repeatable, tracible and relevant evaluation of wound healing, in addition to the typical 2D-perspective that most of the clinical trials use,” says Mia Phillipson, SciLifeLab co-director and professor at Uppsala University.
A total of 240 induced wounds were induced and examined in the 36 healthy volunteers of the study.
The results show that treatment with ILP100-Topical was safe and well tolerated at all doses, and neither ILP100 nor CXCL12 was detectable in places other than the wounds. A significantly larger proportion of healed wounds (p=0.020) were observed on day 32 following multi-dosing with ILP100-Topical compared to saline solution and placebo (76% (73/96) versus 59% (57/96) healed wounds) when the results from all doses of ILP100-Topical were combined. Moreover, the time to first registered healing was reduced by an average of 6 days, and by 10 days at the highest dose. The mode of action of ILP100-Topical was also confirmed, as the treatment resulted in increased CXCL12-positive cells in the wounds and increased blood flow around the wounds during the healing phase.
“Our study shows that bacteria modified to produce and deliver human proteins for local effects can be used as drugs to accelerate wound healing. This is the first time this has been shown in a randomized and placebo-controlled clinical trial. Also, these results are from healthy subjects with functional wound repair mechanisms – the effect size is expected to be greater in patients with diseases that negatively affect wound healing,” says Mia Phillipson.
The advantageous safety profile and the observed beneficial effects on wound healing support the continued clinical development of ILP100-Topical for treating complicated and chronic wounds in patients, which is already underway.
Many immunologically active proteins are naturally unstable with a short biologic half-life. Engineering lactic acid bacteria to produce and release these proteins at the site of action is a clever and feasible way to develop them as pharmaceuticals.
“The potential is practically limitless when you consider the critical role proteins play in various processes in the body and how many diseases still have unmet medical needs not covered by today’s treatments. Based on the same technology platform used for ILP100-Topcial we have created a second drug candidate to revert inflammation and heal ulcers in the intestine of cancer patients treated with immune check-point inhibition. It’s called ILP100-Oral. Shortly we will be initiating a research project where another chemokine is delivered through the same platform for the intended treatment of lung diseases,” says Mia Phillipson.

The SITU-SAFE trial is an adaptive, randomized, double-blind, placebo-controlled, phase 1 study (EudraCT 2019-000680-24) consisting of a first part where increasing doses were given at one time to each participant (SAD), and a second part where multiple and increasing doses were given to each participant (MAD). Both parts of the study consisted of three dose cohorts each. In total, 240 wounds were induced on the upper arms of 36 healthy volunteers, of which 4 wounds (2/arm) in 12 participants in the SAD part, and 8 wounds. Ilya Pharma was founded to develop this new technology into drugs benefitting patients with inadequate treatment alternatives, and is the sponsor of the study.
Read the press release from 2018 about earlier phases of the research.
For more information, contact Mia Phillipson, phone: 018-471 4419, 070-345 50 72, email: Mia.Phillipson@mcb.uu.se.
Emelie Öhnstedt, Evelina Vågesjö, Andreas Fasth, Hava Lofton Tomenius, Pia Dahg, Sofia Jönsson, Nisha Tyagi, Mikael Åström, Zhanar Myktybekova, Lovisa Ringstad, Margareth Jorvid, Peter Frank, Per Hedén, Stefan Roos, Mia Phillipson (2023) Engineered bacteria to accelerate wound healing: an adaptive, randomised, double-blind, placebo-controlled, first-in-human phase 1 trial, eClinicalMedicine.
DOI: 10.1016/j.eclinm.2023.102014
Uppsala University press release (in Swedish)