Novel molecular microscopy uncovers breast cancer spread
In an international collaboration, Mats Nilsson (SU), SciLifeLab researcher and Platform director of the Spatial and Single Cell Biology Platform, have developed a new kind of microscopy, which can map the growth of breast cancer in unprecedented detail. Their study calls attention to how specifically the cells surrounding tumors might be used to control the spread of disease.
In the UK, breast cancer is the most common cancer type, with around 55 870 people (370 men) diagnosed each year. Uncontrollable cell growth due to mutations is the cause of breast cancer. As the growth progresses, it becomes a “patchwork of cells” called cancer clones, carrying different mutations. Since they differ, each clone may not respond in the same way to treatments, with some spreading and others becoming resistant.
In a collaboration between SciLifeLab, the Wellcome Sanger Institute, EMBL’s European Bioinformatics Institute (EMBL-EBI), the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ), and other collaborators – a novel technology, able to trace which specific populations of breast cancer cells are responsible for disease, has been developed.
The study, published in Nature, details their advances in mapping tumor development by combining the genetic information of cancer cells and changes in their gene expression, with surrounding cell types and their interactions with the local environment over time.
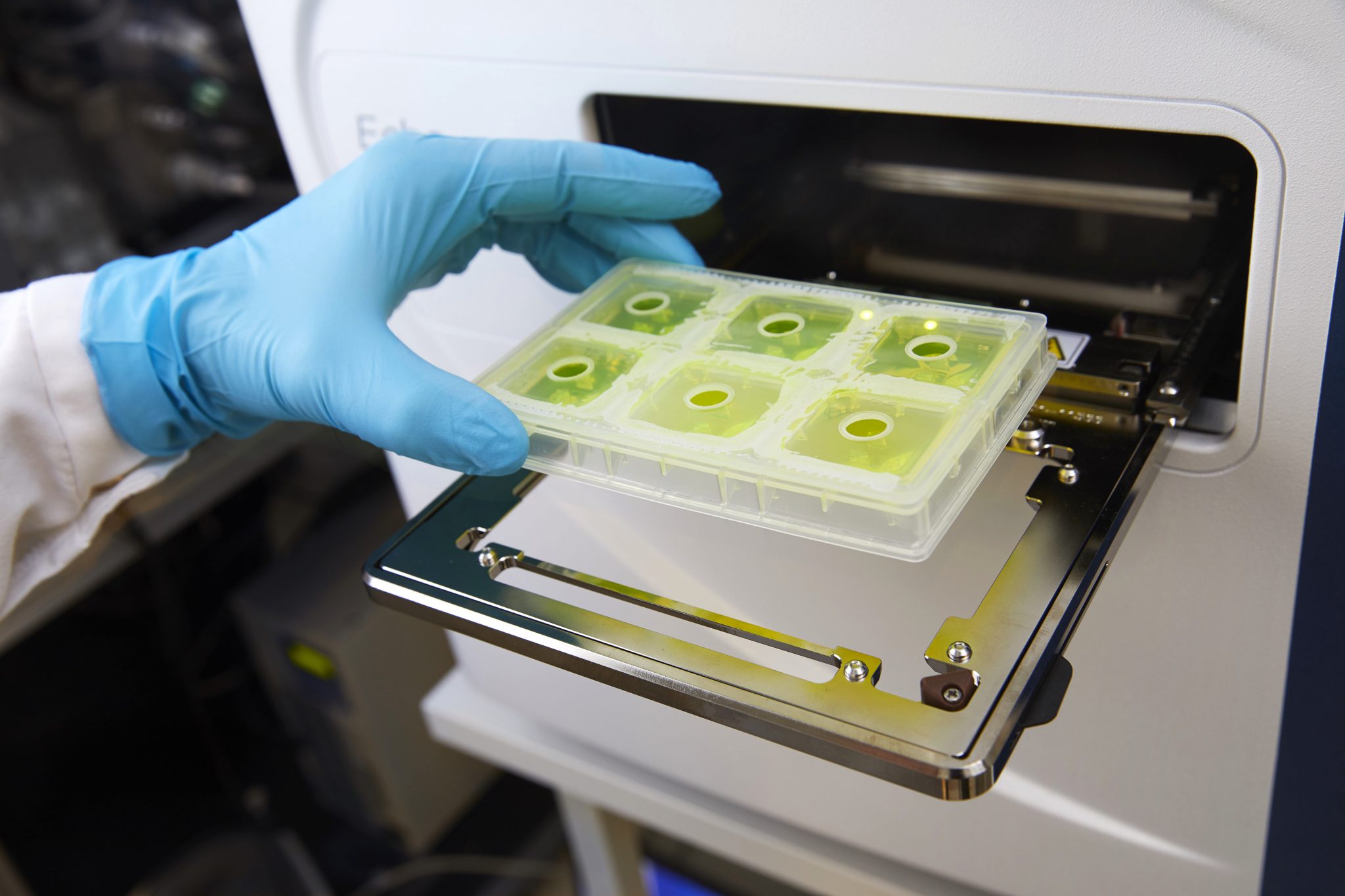
This is done by using several hundred thousand very small fluorescent molecular probes to enter and extract data from cellular DNA and RNA, and scan big tissue areas with fluorescence microscopy.
“Cancer is caused by genetic mutations in a cell, and this was the first time that we were able to use DNA base-specific probes to target dozens of these mutations in a set of cancer cell clones. This innovative technique allowed us to accurately reconstruct the spread of these clones”, says co-last author Mats Nilsson, in a press release from the Wellcome Sanger Institute.
According to the press release, the occurrence of individual mutations is influenced by the activities, cells, and immune system surrounding the cancer cells. By tracking which specific mutations occur, which cancer cells migrate to other parts of the body, and their environment – the researchers can build a complete picture of the tumor evolution.
“An important insight from our research is that it may not be the genetic changes alone that are the reason that the cancer cells survive and spread; it could also be where they are. This adds another layer of complexity as well regarding new potential ways to target the disease. It may also offer explanations about why some treatments only work in some individuals, even if they have similar mutations to others, as the tumors are found in different areas of the breast”, says Mats Nilsson.
The research may lead to a future development in which therapies can mitigate cancer growth and spread, by targeting its environment. The new tool could also be used to monitor and test how different treatments affect the cancer as well as its interaction with the surrounding immune system simultaneously, which can give a more complete picture of therapies and their side effects.
“Sequencing cancer tumors can give us a good understanding about the genetic diversity in a tumor. But the exciting thing about this technology is that for the first time, we can see how the environment shapes cancer evolution. By not only being able to see which cancer clones progress to become more aggressive, but also which didn’t, it will enable us to get a much better understanding of what the key steps are in tumor growth, and how we can lessen or prevent disease”, says co-last author Moritz Gerstung from the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ).
“Our research has created a tool that can trace which breast cancer cells go on to cause tumors in other parts of the body, and can help answer some of the big questions in cancer, such as why some cancer cells spread and some don’t. To fully understand and therefore treat breast cancer, we need to be able to see the entire picture of how the cancer interacts in the body, with the cells around it, and with the immune system. This new technology combines multiple techniques and expertise to do this, bringing together different approaches to give a complete view of cancer that has not been previously possible”, says co-senior author Lucy Yates from the Wellcome Sanger Institute.