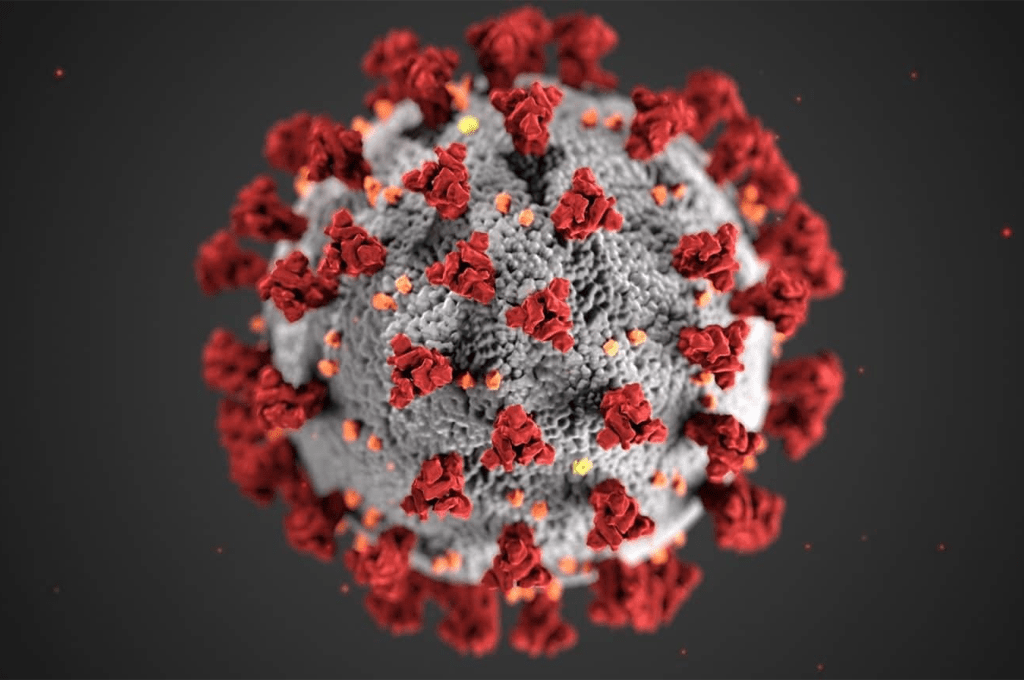
Investigating mucosal immunity: Key insights for SARS-CoV-2 vaccine development
Several novel vaccine platforms are now focusing on enhancing mucosal immunity in the respiratory tract to combat the transmission of SARS-CoV-2. However, for effective comparison across different vaccine trials and real-world scenarios, standardized methods for collecting mucosal samples and quantifying mucosal antibodies are urgently needed.
This research is a component of the COMMUNITY study, funded by the National SciLifeLab-KAW COVID-19 Research Program.
In this study, an international team of researchers analyzed SARS-CoV-2 spike-specific IgA and IgG levels in saliva, nasal secretions, and serum samples from 1048 SARS-CoV-2 vaccinated healthcare workers enrolled in the COMMUNITY study at Danderyd Hospital, both with and without prior SARS-CoV-2 infection, using commercial electrochemiluminescence antibody panels.
“Since the choice of collection technique and sampling localization could introduce variations and confounding factors, we saw a great need for a head-to-head comparison of SARS-CoV-2 antibodies in saliva and nasal secretions,” says Mikael Åberg associate professor and head of Affinity Proteomics at SciLifeLab and Uppsala University
The findings revealed strong correlations between spike-specific IgA levels in nasal secretions and saliva, but the levels were more than three times higher in nasal secretions compared to saliva. Additionally, spike-specific IgA showed stronger correlations between serum and saliva samples, indicating the transudation of monomeric spike-specific IgA from the bloodstream to saliva.
Notably, spike-specific dimeric secretory IgA (SIgA) demonstrated significantly higher cross-binding capacity to SARS-CoV-2 variants compared to monomeric spike-specific IgA and IgG in all mucosal secretions, underscoring the importance of considering serum-derived monomeric IgA when investigating mucosal correlates of protection against infection.
The results suggest that while spike-specific IgA can be reliably measured in both nasal secretions and saliva, nasal secretions may offer advantages with higher levels and likely a larger proportion of protective dimeric SIgA. Moreover, the superior variant cross-binding capacity of dimeric SIgA in mucosal secretions highlights the potential protective benefits of vaccines targeting the upper respiratory tract. These insights are crucial for optimizing vaccine strategies against SARS-CoV-2 transmission.
“Mucosal vaccines could be a gamechanger in preventing infections and viral spread by eliciting immune responses directly at the site of viral entry – the respiratory mucosa. Several mucosal vaccines are therefore in development, but we lack standardized methods to validate the immune responses they generate. Our findings are a first step towards establishing uniform protocols for mucosal sampling and the quantification of antigen-specific IgA in nasal secretions,” says Charlotte Thålin, docent at Karolinska Institutet, the Department of Clinical Sciences, Danderyd Hospital, and principal investigator of the COMMUNITY study.
This study was supported by grants from the Jonas and Christina at Jochnick Foundation, Region Stockholm, SciLifeLab, the Knut and Alice Wallenberg Foundation, the Leif Lundblad Family Foundation, the Swedish Research Council, the Swedish Heart and Lung Foundation, the Bill & Melinda Gates Foundation, and the Center for Innovative Medicine.