When symptoms are vague, proteins can point the way
SciLifeLab technology helped power a new Nature Communications study that moves blood-based cancer triage closer to real-world care.
A person arrives at a clinic feeling unwell, unusually tired, losing weight, maybe running a low fever that won’t go away. It’s the kind of appointment that can be unsettling for both patient and clinician, because the symptoms are real, but they don’t clearly “belong” to any one organ. It might be an infection. It might be an autoimmune flare. It might be something inflammatory. Or, in the worst case, it might be cancer. This clinical grey zone is where modern diagnostics often struggle. Advanced imaging and biopsies can be highly informative, but they are also resource-intensive.
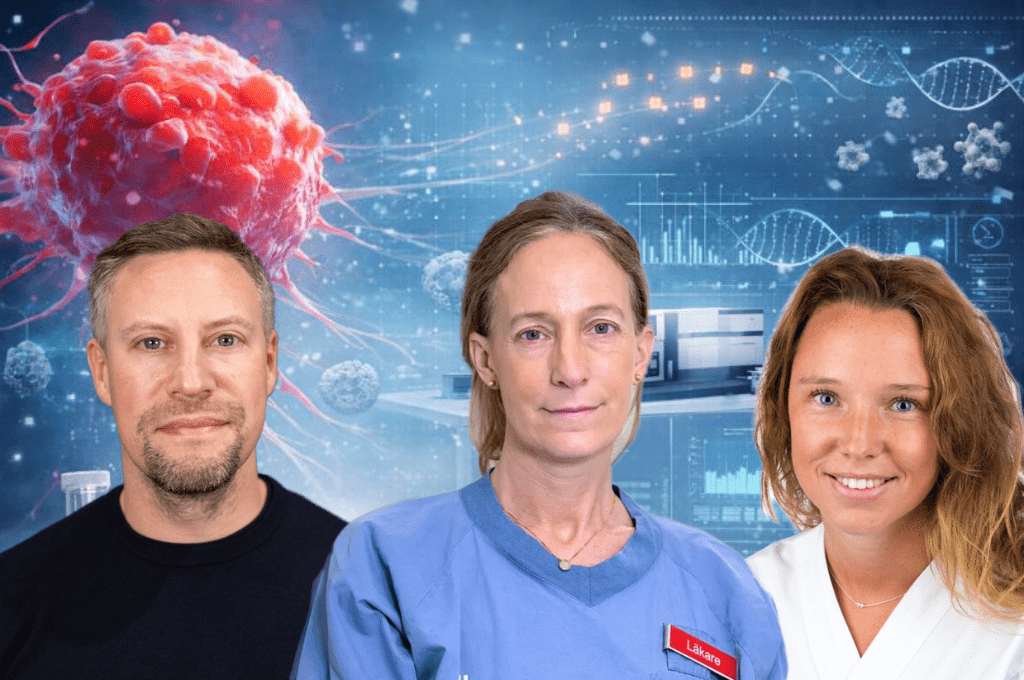
Now, SciLifeLab research reports a step toward a practical solution: using a single blood sample to read a “protein pattern” that can help identify which patients with non-specific symptoms are more likely to have an underlying cancer, and which patients may be more likely to have other non-cancer conditions. The study, led by researchers at Karolinska Institutet, Danderyds Sjukhus (KI DS) and SciLifeLab Uppsala in collaboration with Örebro University and KTH Royal Institute of Technology, has been published in Nature Communications.
This study focuses on something immediately actionable: triage for symptomatic patients — helping clinicians decide who should be prioritized for fast, advanced diagnostic work-ups, and who might avoid unnecessary and potentially stressful investigations.
“When patients seek healthcare because they feel unwell but have no clear, organ-specific symptoms, it can be difficult to determine whether cancer is the cause. Our research asks whether patterns of proteins in a single blood sample can help identify which patients with vague symptoms are more likely to have an underlying cancer, and which patients are more likely to have other non-cancer conditions,” says Fredrika Wannberg, resident at Danderyd Hospital and doctoral student at the Department of Clinical Sciences, Danderyd Hospital, Karolinska Institutet.
DNA is often described as a blueprint. But proteins are closer to the body’s live status updates. They change when the immune system is activated, when tissues are inflamed, when infections take hold, and when cancers grow and interact with the body.
Proteomics, the large-scale measurement of proteins, has expanded rapidly in recent years. In this study, researchers measured the levels of 1,463 proteins using Olink’s proximity extension assay (PEA), paired with next-generation sequencing readout on an Illumina NovaSeq . The model they built was designed not as a replacement for imaging or biopsies, but as a way to decide who should get those next steps sooner.
“The study shows the potential of large-scale proteomics for extracting clinically relevant information from small amounts of blood,” says co-author Mikael Åberg, associate professor at Uppsala University and head of SciLifeLab Affinity Proteomics Uppsala, the unit where the proteomic analyses were performed.
The team, led by Charlotte Thålin, adjunct Professor at Karolinska Institutet and Senior Consultant at Danderyd Hospital, worked with blood samples from patients who had been referred to fast-track diagnostic pathways for non-specific symptoms suggestive of cancer. Importantly, the blood samples were taken before the full diagnostic work-up began. That timing is crucial: it mirrors the moment in healthcare where decisions are hardest, and where a triage tool would be most valuable.
In total, samples from 694 patients across two cohorts were analyzed: a discovery cohort of 456 patients from the Diagnostic Center at Danderyds sjukhus and an independent replication cohort of 238 patients from the Diagnostic Center at Örebro University Hospital. To help interpret what the strongest protein signals might mean biologically, the team, cross-referenced findings with annotations from the Human Protein Atlas, which maps where proteins are typically expressed in the body and highlights proteins linked to cancer.
“We found that specific patterns of proteins in blood differ between patients who were later diagnosed with cancer and those who were not. Using plasma protein profiling, we developed a model that could distinguish cancer from non-cancer with good performance, even when the non-cancer patients were later diagnosed with inflammatory, autoimmune or infectious diseases.
This is important because these conditions often resemble cancer both clinically and biologically, making diagnosis especially challenging. Our findings suggest that information from a single blood sample could help clinicians decide which patients should be prioritized for further cancer investigations.” says Mikael Åberg
Beyond instruments and assays, a key part of the research was how SciLifeLab was able to act as a meeting point by connecting clinical cohorts, analytical capacity, and data science expertise into a single workflow.
As Mikael Åberg explains, “The collaboration between SciLifeLab Affinity Proteomics and NGI in Uppsala to set up and run proteomics with an NGS-based read-out made it possible to generate high-quality proteomic data from a large and clinically complex patient cohort, which was essential for developing and validating the predictive model. By also functioning as a coordinating nexus within the research network, the unit linked us to a second group, led by ScilLifeLab Group Leader Gisela Helenius, that supplied a validation cohort and to a third group with SciLifeLab/KTH PhD student María Bueno Álvez that contributed further expertise in statistical analysis.”
Measuring proteins is only the beginning. “The next step is further validation of the findings in additional patient groups, particularly in primary care settings where cancer prevalence is lower. We also aim to refine the protein panel to make future tests simpler and more suitable for clinical implementation. Ultimately, the goal is to evaluate whether this approach can support routine clinical decision-making,” Charlotte Thålin concludes.